Date : Nov 4 , 2025 |
Coronary Artery Bypass Grafting is a surgical procedure, in which blocked or narrowed coronary arteries are bypassed with blood vessels, taken from other parts of the body, so that normal blood flow to the heart muscle can be restored.
This procedure is generally recommended for patients affected by severe coronary artery disease, angina (chest pain), or multiple blockages in the heart’s arteries that limit the supply of oxygen-rich blood to the heart muscle.
This surgery, significantly relief chest pain, reduce risk of the heart attack, improve heart function, and restore patient’s ability to carry out daily activities.
During this surgery, healthy blood vessel is taken from the leg, chest, or arm and connect to the coronary artery beyond the site of blockage, allowing a new pathway for blood to flow. After the surgery, patient is closely monitored, and cardiac rehabilitation with lifestyle modifications is advised to ensure complete recovery and long-term heart health.
Traditional On-Pump CABG Surgery
This is the most common type of coronary artery bypass surgery, performed with the assistance of a heart-lung machine (cardiopulmonary bypass). During the procedure, the heart is temporarily stopped, and the heart-lung machine is used to take over the function of pumping blood and supplying oxygen throughout the body while the bypass grafting is carried out.
A high success rate of about 95–98% has been reported with this surgery, most of the patient relief from chest pain and an improved quality of life. A large incision is made down the center of the chest (sternotomy) to access the heart. Once the grafts are attached, the heart is restarted, and the patient is gradually weaned off the heart-lung machine.
A modern technique, that aims to achieve the same results as traditional CABG but without stopping the heart or using a heart-lung machine. This technique allows the surgeon to perform bypass grafting on a beating heart, using specialized stabilization devices that hold a small area of the heart, while the rest continues to beat.
This surgery requires exceptional skill and experience of the surgeon, as they work on a moving target with limited stabilization. Among the most important advantages of this procedure are reduced risk of stroke, less blood loss, decreased inflammation, shorter hospital stay, and faster recovery compared to on-pump surgery.
This technique is particularly beneficial for high-risk patients, elderly patients, or those with kidney disease or previous stroke. Most patients experience fewer complications and can return to daily activities faster, though not all patients are suitable candidates for this approach.
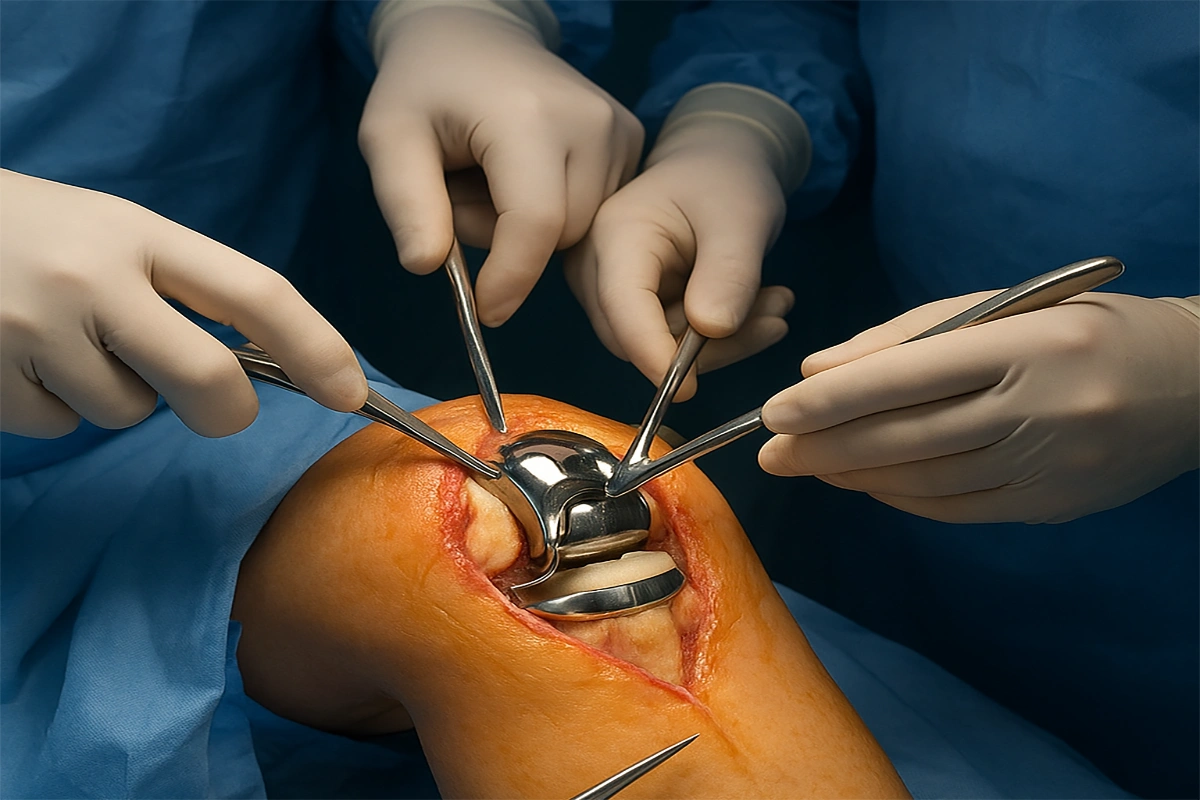
An advanced technique, that uses smaller incisions instead of the traditional full sternotomy. The surgeon accesses the heart through a small incision between the ribs on the left side of the chest, typically to bypass blockages in the front of the heart.
During this operation, specialized instruments and robotic assistance are used to perform the bypass through smaller incisions. This technique is usually performed off-pump (on a beating heart), and primarily uses the internal mammary artery from inside the chest wall as the graft.
The benefits of this technique include less surgical trauma, reduced pain, smaller scars, faster recovery, shorter hospital stay, and quicker return to normal activities. Patients typically experience less blood loss and reduced risk of infection. However, this technique is suitable only for specific blockages and not all patients are candidates. The surgeon must carefully evaluate the location and severity of blockages to determine if MIDCAB is appropriate.
A cutting-edge technique, that uses a robotic surgical system to achieve superior precision in performing bypass grafting through very small incisions. The robotic system provides the surgeon enhanced three-dimensional visualization, and instruments with greater dexterity and range of motion more than the human hand.
During the operation, the surgeon sits at a console and controls robotic arms, that hold specialized instruments and a high-definition camera. The robot translates the surgeon’s hand movements into precise micro-movements inside the chest, eliminating natural hand tremors, and allowing for extremely accurate suturing of the tiny coronary arteries.
The benefits of this technique include minimal scarring, reduced pain and trauma, less blood loss, lower infection risk, shorter hospital stay, and faster return to work and normal activities.
Studies indicate that patients who undergo robotic CABG often experience excellent graft patency rates and outcomes comparable to traditional surgery, with the added benefits of minimally invasive approach. However, this technology requires significant investment and specialized training, making it available only at advanced cardiac centers.
CABG surgery is recommended when there is severe coronary artery disease with significant blockages that don’t respond adequately to medications or lifestyle changes, particularly when multiple arteries are blocked or the left main coronary artery is affected. It is also indicated for severe angina (chest pain) that limits daily activities such as walking, climbing stairs, or performing household tasks, or when previous interventions like angioplasty or stenting have failed or are not suitable options.
In such cases, conservative treatments are first attempted, including medications (blood thinners, cholesterol-lowering drugs, blood pressure medications), lifestyle modifications (diet, change, smoking cessation), and weight management. However, when these fail to provide adequate relief or when the blockages are too severe or extensive, CABG becomes necessary. Age is typically considered when patients are experiencing symptoms that significantly impact their quality of life, sleep, and overall health due to heart disease.
CABG surgery is performed to restore adequate blood flow to the heart muscle, relieve severe angina (chest pain), reduce the risk of heart attack, and improve survival in patients suffering from severe coronary artery disease. The surgery is typically recommended after medical therapy alone has proven insufficient to control symptoms, or when the pattern of blockages poses a high risk for heart attack or sudden death.
During the procedure, the surgeon harvests healthy blood vessels from the leg (saphenous vein), chest (internal mammary artery), or arm (radial artery) and uses them to create detours around the blocked segments of coronary arteries. This allows oxygen-rich blood to reach the heart muscle beyond the blockages, restoring proper cardiac function.
This surgery helps relieve chest pain, improve exercise tolerance, reduce shortness of breath, and enable the patient to perform daily activities normally without cardiac limitations.
Choosing the right surgeon: Ensure you select a highly skilled cardiac surgeon with extensive experience, and proven track record that has in CABG procedures at a reputable cardiac center.
Selecting a specialized hospital: Verify that the hospital has an advanced cardiac ICU, experienced nursing staff, and comprehensive cardiac care program
Adhering to preoperative instructions: Follow all medical guidelines precisely, including medication adjustments, fasting requirements, and skin preparation
Strict medication compliance: Take all prescribed medications exactly as directed, especially blood thinners, beta-blockers, and cholesterol medications
Following sternum precautions: Protect the breastbone while healing by avoiding pushing, pulling, or lifting more than 5-10 pounds for 6-8 weeks
Gradual activity increase: Slowly increase physical activity as directed, avoiding sudden exertion or overexertion
Maintaining nutrition and hydration: Follow a heart-healthy diet low in sodium and saturated fats, with adequate protein for healing
Regular follow-up: Attend all scheduled appointments and undergo recommended cardiac testing
Cardiac rehabilitation participation: Enroll in and actively participate in supervised cardiac rehabilitation program
Early detection of complications: Immediately report any warning signs such as chest pain, shortness of breath, fever, wound drainage, irregular heartbeat, or leg swelling
Infection prevention: Keep incisions clean and dry, wash hands frequently, and avoid crowds during initial recovery
Smoking cessation: Absolutely no smoking, as it dramatically increases risk of graft failure and complications
Stress management: Practice relaxation techniques and get adequate rest to support healing
Monitoring vital signs: Regularly check and record blood pressure, heart rate, and weight as instructed
1- Relief from Angina (Chest Pain)
2- Improved Exercise Tolerance and Physical Function
3- Reduced Risk of Heart Attack
4- Improved Survival and Life Expectancy
5- Restoration of Quality of Life
6- Improved Heart Function
7- Better Sleep and Reduced Anxiety
8- Return to Work and Productive Life
9- Reduced Medication Burden
10- Long-term Graft Patency
11- Comprehensive Protection
Unlike angioplasty with stenting, which typically treats only one blockage at a time, CABG can bypass multiple blockages simultaneously, providing comprehensive revascularization and protection for the entire heart. This “complete” treatment approach is particularly valuable for patients with diffuse, multi-vessel disease.
Is CABG surgery painful?
CABG surgery is a major surgery, so some discomfort is expected, but pain is very manageable with modern pain management techniques. Pain gradually decreases over the first 2-3 weeks and is usually minimal by 4-6 weeks.
What is the success rate of CABG surgery?
CABG surgery success rate is 95 to 99% in most patients. The operative mortality rate is typically 1-2% for standard-risk patients, though this can be higher for emergency cases, elderly patients, or those with multiple comorbidities.
Success depends on multiple factors including surgeon’s experience, patient’s age and health conditions, number of grafts needed, presence of complications, and patient compliance with medications and lifestyle changes after surgery. At specialized cardiac centers with experienced teams, outcomes are typically excellent.
How long does it take to recover from CABG surgery?
Hospital recovery takes 5-7 days for uncomplicated cases, Once home, you’ll need 4-6 weeks, during which, you’ll gradually increase activity and begin cardiac rehabilitation. Most patients can return to light work and driving by 6-8 weeks, though strenuous jobs may require 8-12 weeks. Full sternum healing takes about 12 weeks (3 months), after which you can resume most normal activities including lifting. Maximal recovery and return to optimal fitness typically takes 4-6 months with cardiac rehabilitation. However, many patients continue to feel progressively better for up to a year.
CABG surgery can be safe for elderly patients, even those over 75-80 years old, though risks are somewhat higher than younger patients. Modern surgical techniques, improved anesthesia, and better postoperative care have made CABG safer for older adults.
Can I resume normal activities after CABG?
Yes, most patients can resume normal activities, and even exceed their pre-surgery activity levels after full recovery from CABG. Once cleared by your doctor (typically at 3-6 months), you can return to most activities including work, household chores, gardening, traveling, sexual activity, and recreational sports. However, some permanent restrictions may apply: avoid heavy lifting and avoid high-impact contact sports that could injure the chest, and avoid extreme physical stress without proper conditioning.
What lifestyle changes are necessary after CABG?
CABG surgery provides mechanical improvement in blood flow, but lifelong lifestyle changes are essential to protect the grafts and prevent progression of coronary disease. Critical changes include: Complete smoking cessation, Heart-healthy diet, Regular exercise, Weight management, Stress reduction, Medication compliance, Blood pressure control, Cholesterol management, Diabetes control, and Regular medical follow-up.
Many CABG patients live the rest of their lives without needing additional heart procedures, especially if they maintain good lifestyle habits and medication compliance. However, some patients may eventually require additional interventions. Approximately 5% of patients may need repeat coronary interventions (angioplasty, stenting, or repeat CABG) within 10-15 years.
What are the risks and potential complications?
While CABG is generally safe with excellent outcomes, like any major surgery, it carries potential risks including:
Date : Dec 12 , 2025
Date : Oct 29 , 2025
Date : Jun 21 , 2025